A nurse is caring for a term macrosomic newborn, a task that demands specialized knowledge and meticulous attention. This guide delves into the intricate care and management strategies for these infants, encompassing assessment, monitoring, potential complications, and long-term outcomes. By exploring the nuances of macrosomic newborn care, nurses can optimize the health and well-being of these vulnerable infants.
Understanding the maternal factors contributing to macrosomia, such as gestational diabetes and obesity, is crucial for risk assessment and early intervention. Assessment techniques like ultrasound measurements and fundal height evaluation aid in identifying macrosomia during pregnancy and delivery. Monitoring for potential complications like hypoglycemia and respiratory distress is essential, with the NICU playing a vital role in managing these infants.
Maternal Factors Contributing to Macrosomia: A Nurse Is Caring For A Term Macrosomic Newborn
Macrosomia is a condition characterized by an abnormally large birth weight, typically defined as a birth weight above the 95th percentile for gestational age. Maternal factors play a significant role in the development of macrosomia.
Gestational diabetes is a major risk factor for macrosomia. Insulin resistance during pregnancy can lead to excessive fetal growth. Women with gestational diabetes are at an increased risk of delivering macrosomic infants, with a risk of up to 25%.
Maternal obesity is another significant contributor to macrosomia. Obese women have higher levels of insulin and other growth factors that can cross the placenta and promote fetal growth. The risk of macrosomia is directly proportional to the degree of maternal obesity, with obese women having a 2- to 3-fold increased risk compared to women with a normal BMI.
Advanced maternal age is also associated with an increased risk of macrosomia. As women age, their insulin sensitivity decreases, which can lead to increased fetal growth. Women over the age of 35 are at an increased risk of delivering macrosomic infants.
Assessment and Monitoring of Macrosomic Newborns
Assessment of macrosomia during pregnancy can be done using ultrasound measurements. Fundal height evaluation can also provide an indication of fetal size.
Macrosomic newborns require close monitoring for potential complications. Hypoglycemia is a common complication in macrosomic infants due to their increased insulin levels. Respiratory distress may also occur due to the increased airway resistance and decreased lung compliance associated with macrosomia.
Birth injuries are another potential complication in macrosomic newborns. The large size of the infant can make delivery difficult, leading to injuries such as shoulder dystocia and brachial plexus palsy.
Macrosomic infants may require specialized care in the Neonatal Intensive Care Unit (NICU). NICU provides a controlled environment with specialized equipment and staff trained to manage the unique needs of macrosomic infants.
Care and Management Strategies for Macrosomic Newborns
Feeding strategies for macrosomic newborns include frequent feedings to prevent hypoglycemia. Kangaroo care, which involves skin-to-skin contact between the infant and the mother, can help regulate the infant’s temperature and promote bonding.
Handling techniques for macrosomic newborns should be gentle and supportive. Specialized equipment, such as isolettes and CPAP machines, may be necessary to provide adequate respiratory support.
Lactation consultants and dietitians play a crucial role in providing guidance and support to mothers of macrosomic newborns. They can assist with breastfeeding and provide nutritional advice to ensure the infant receives adequate nourishment.
Potential Complications and Long-Term Outcomes
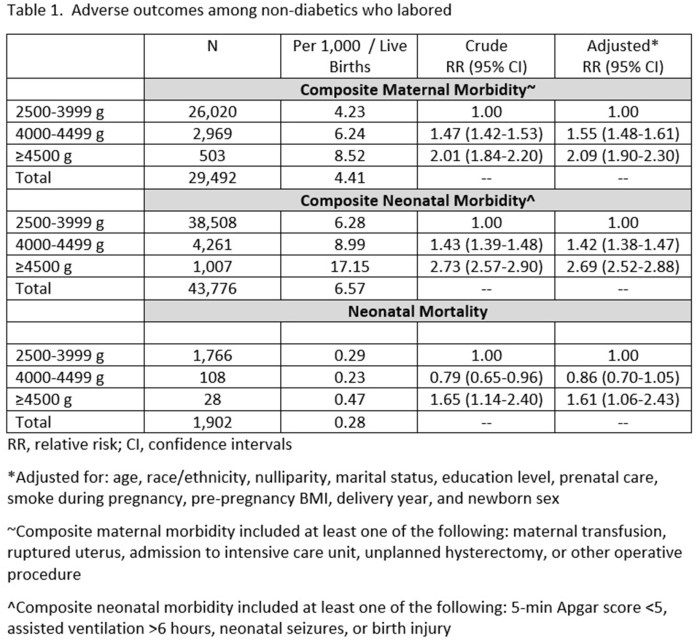
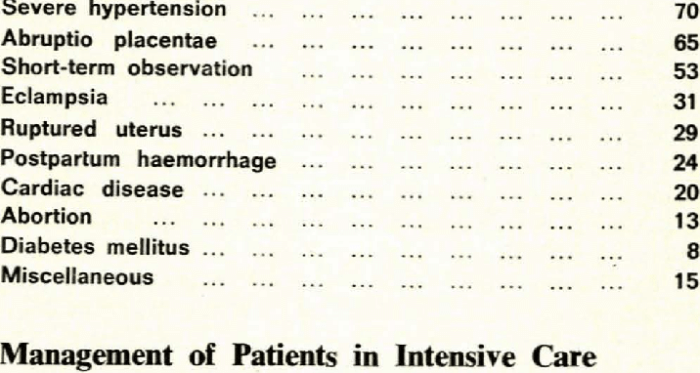
Potential complications associated with macrosomia include birth injuries, respiratory distress, and metabolic disorders. Birth injuries can range from minor abrasions to more serious injuries such as fractures and nerve damage.
Respiratory distress can occur due to the increased airway resistance and decreased lung compliance associated with macrosomia. Metabolic disorders, such as hypoglycemia and hyperglycemia, can also occur due to the altered glucose metabolism in macrosomic infants.
Long-term outcomes of macrosomic newborns include an increased risk of obesity, diabetes, and cardiovascular disease. Macrosomic infants are more likely to develop metabolic syndrome, which is a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes.
Follow-up care and monitoring of macrosomic infants are essential to optimize their health and well-being. Regular checkups with a healthcare provider can help identify and address any potential complications.
Questions Often Asked
What are the common feeding challenges faced by macrosomic newborns?
Macrosomic newborns may experience difficulty latching due to their large size and immature sucking reflex. They may also be at risk for aspiration due to their underdeveloped gag reflex.
How can nurses promote skin-to-skin contact for macrosomic newborns?
Nurses can encourage skin-to-skin contact by placing the newborn on the mother’s chest immediately after birth and supporting the mother in holding the newborn in an upright position for extended periods.
What are the signs and symptoms of hypoglycemia in macrosomic newborns?
Signs and symptoms of hypoglycemia in macrosomic newborns include jitteriness, lethargy, poor feeding, and seizures.